STDCHECK.COM
10-TEST PANEL
To be STI and STD free, every person must adhere to very good health instructions, precautions, preventions, regualar diagnoses, especially when expose or unsure of your sexual patners and complete available treatment. The following are some of the common STDs that can affect an individual is necessary measures are not taken to prevent them, their preentive measure, diagnoses and available treatment.
GONORRHEA: CAUSES, SYMPTOMS AND DIAGNOSIS
What is gonorrhea? What are the first noticeable sign?
Gonorrhea is a sexually transmitted infection (STI) caused by the Neisseria gonorrhoeae bacterium. It affects the mucous membranes of the reproductive tract, including the cervix, uterus, fallopian tubes in women, and the urethra in both men and women. Understanding gonorrhea is crucial due to its high prevalence and potential severe health complications if left untreated. The gonorrhea bacteria are most often passed from one person to another during sexual contact, including oral, anal or vaginal intercourse.
First Noticeable signs of Gonorrhea in men:
If you get symptoms, they usually start 3 to 8 days after you’ve been exposed to chlamydia germs. The symptoms may be mild. Common symptoms in men include: painful urination, white, yellow, or green urethral discharge, and swollen testicles, pain or burning sensation when urinating and thick, fever, cloudy or bloody discharge from the penis.
First Noticeable signs of Gonorrhea in women:
If you get symptoms, they usually start 5 to 14 days after you’ve been exposed to chlamydia germs. The symptoms may be mild. painful urination, which may feel like burning, pain in the lower part of the stomach area, also called the abdomen, lower back pain, fever, vaginal discharge, vaginal pain during sex, bleeding between periods, testicle pain or swelling, rectal pain, discharge or bleeding Women may experience milder symptoms, leading to underdiagnosis. However, women are at a higher risk of severe complications like pelvic inflammatory disease (PID), which can result in infertility if untreated.
Only medical diagnosis guarantees one safety. Click now to book an appointment or see a doctor
CAUSES AND RISK FACTORS OF GONORRHEA
Causes and risk factors include biological factors, environmental factors, lifestyle factors, and lifestyle factors. Diagnosis involves urine tests and swabs of affected areas. Common diagnostic tools include nucleic acid amplification tests (NAATs) and culture tests. Misdiagnosis issues can occur due to overlapping symptoms with other STIs or infections.
GONORHEA DIAGNOSIS AND TREATMENT
Treatment options include antibiotics, but antibiotics must be administered, only after a thorough medical diagnosis, to avoid uncertainties and complications, supportive treatments, lifestyle adjustments, and regular check-ups. Preventive measures include consistent use of condoms during sexual activity, limiting sexual partners, and regular STI screenings. Safe practices, such as using dental dams for oral sex and ensuring mutual monogamy with an uninfected partner, significantly reduce the risk of gonorrhea.
Call To Action
Late diagnoses and laboratory test is often life threatening and dangerous. Early diagnoses saves life and it highly advantageous. Go run that test now! STDCHECK.COM
MEDICAL EXPERTS RECOMMENDATIONS
Health experts recommend regular screenings and open communication with sexual partners about STI status to reduce the risk of gonorrhea and other STIs.
HERPES 1 AND 2
KEY FACTS ABOUT HERPES
According to WHO facts on Herpes;
- An estimated 3.7 billion people under age 50 (67%) globally have herpes simplex virus type 1 (HSV-1) infection, the main cause of oral herpes.
- An estimated 491 million people aged 15–49 (13%) worldwide have herpes simplex virus type 2 (HSV-2) infection, the main cause of genital herpes.
- Most HSV infections are asymptomatic or unrecognized, but symptoms of herpes include painful blisters or ulcers that can recur over time.
- Infection with HSV-2 increases the risk of acquiring and transmitting HIV infection.
Human alphaherpesvirus 2 or Herpes simplex virus 2 is a species of virus in the genus Simplexvirus, subfamily Alphaherpesvirinae, family Herpesviridae, and order Herpesvirales. Scientific name: Human herpesvirus 2 and the Genus: Simplexvirus.
Genital herpes is essentially a minor, sometimes recurring, skin infection; ‘cold sores’ which occur on the genitals rather than the face. It does not cause long-term ill health or affect longevity of life. People who get genital herpes can and do lead perfectly normal lives.
SIGNS AND SYMPTOMS OF HERPES 1 AND 2
Herpes is a common infection that can cause painful, recurring blisters or ulcers. Symptoms can vary from the first episode to recurrent episodes, these include: fever body aches sore throat (oral herpes) headache swollen lymph nodes near the infection. Common oral and genital herpes symptoms include cold sores or open sores, while recurrent outbreaks are shorter and less severe. Medications can reduce symptoms but cannot cure the infection. Recurrent symptoms can be distressing and stigmatizing, impacting sexual relationships. Eventually, most people with herpes adjust to living with the infection.
Having the knowledge that Herpes can only be treated and not parmanetly cured, how then do you know if you have contracted it or not, your health status, the right suitable drugs to use, and help or advice from the expert? CLICK HERE!
GET TESTED FOR HSV 1 AND HSV 2
TRANSMISSION OF HSV 1 AND HSV 2
“HSV-1 is mainly transmitted via contact with the virus in sores, saliva, or surfaces in or around the mouth. Less commonly, HSV-1 can be transmitted to the genital area through oral-genital contact to cause genital herpes. It can be transmitted from oral or skin surfaces that appear normal; however, the greatest risk of transmission is when there are active sores. People who already have HSV-1 are not at risk of reinfection, but they are still at risk of acquiring HSV-2.
HSV-2 is mainly transmitted during sex through contact with genital or anal surfaces, skin, sores or fluids of someone infected with the virus. HSV-2 can be transmitted even if the skin looks normal and is often transmitted in the absence of symptoms.
In rare circumstances, herpes (HSV-1 and HSV-2) can be transmitted from mother to child during delivery, causing neonatal herpes”. Credited to https://www.who.int/news-room/fact-sheets/detail/herpes-simplex-virus
Most people with HIV infections are commonly infected with HSV.
FOLLOW THE SIMPLE TEST BELOW TO GET TESTED ON STDCHECK PLATFORM, BY CLICKING ON THE IMAGE BELOW:
HEPATITIS A, B, AND C
HEPATITIS A
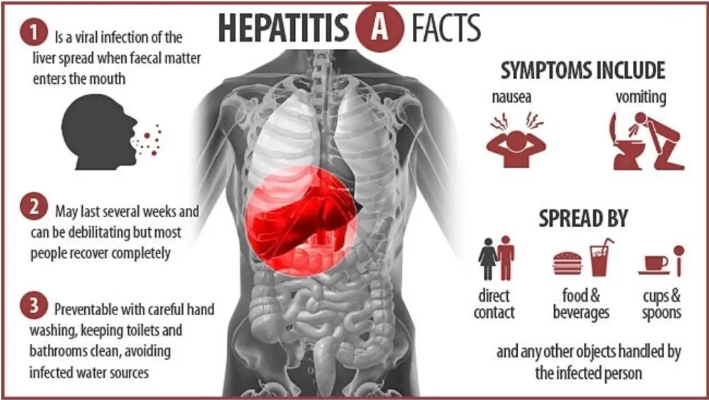
Hepatitis A is a liver-related infectious disease caused by Hepatovirus A (HAV), with symptoms typically lasting 8 weeks and affecting 10-15% of people within 6 months. The virus is spread through contaminated food or drinking water, particularly undercooked or raw shellfish, and close contact with an infectious person. Diagnosis requires blood testing, as symptoms are similar to those of other diseases. Hepatitis A is one of five known hepatitis viruses, and the hepatitis A vaccine is effective for prevention. Other preventive measures include hand washing and proper cooking. No specific treatment is available, but infections usually resolve without ongoing liver disease. treatment for acute liver failure is liver transplantation. Globally, 1.4 million symptomatic cases occur each year and 114 million infections occur, with poor sanitation and unsafe water being more common. In developing countries, 90% of children are infected by age 10 and become immune by adulthood. Acute hepatitis A resulted in 11,200 deaths in 2015. World Hepatitis Day is celebrated annually on July 28 to raise awareness about viral hepatitis.
FOR MORE INFORMATION PLEASE CLICK THE LINK
HOW DO HEPATITIS A TRANSMIT? WHAT ARE THE POSSIBLE CAUSES?
The hepatitis A virus is transmitted primarily by the faecal-oral route; that is when an uninfected person ingests food or water that has been contaminated with the faeces of an infected person. In families, this may happen though dirty hands when an infected person prepares food for family members
The hepatitis A virus (HAV) is commonly found in areas with inadequate sanitation and high population density. It is disseminated by fecal-oral pathways. Parenterally, but less frequently, it can also be spread by blood and blood products. Food-borne illnesses frequently occur, and eating contaminated shellfish puts you at risk for infection. HAV withstands temperatures as high as 60°C, drying, detergent, acid, and solvents. Both fresh and salt water may support it for several months. Children in impoverished nations are frequently infected, yet this can lead to lifetime immunity. Chlorine treatment, formalin, peracetic acid, beta-propiolactone, and ultraviolet light can all render the virus inactive. The majority of vulnerable young adults in wealthy nations who get the illness while traveling to nations with high
EARLY SIGNS AND SYMPTOMS OF HEPATITIS A
Hepatitis A infection can be mistaken for influenza, but some people, especially children, do not show symptoms. Symptoms and signs usually appear 2–6 weeks after the initial infection, with an average of 28 days between infection and symptoms. The risk for symptomatic infection is directly related to age, with over 80% of adults having symptoms compatible with acute viral hepatitis and most children having asymptomatic or unrecognized infections. Symptoms usually last less than 2 months, but some can be ill for up to 6 months. Extrahepatic manifestations include joint pains, fatigue, fever, Nausea,Jaundice (a yellowing of the skin or the whites of the eyes owing to hyperbilirubinemia), Bile being removed from the bloodstream and excreted in the urine, giving it a dark amber color, Diarrhea, Light or clay-colored faeces (acholic faeces), Appetite loss, red cell aplasia, pancreatitis, and generalized lymphadenopathy. Kidney failure and pericarditis are rare, show an acute onset and disappear upon disease resolution.
DON’T WAIT! ARE YOU AT RISK OF ANY OF THE CAUSES OF HEPATITIS A, PLEASE CLICK ON THE LINK
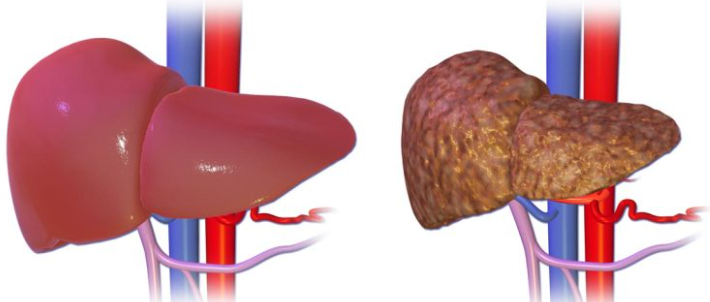
HEPATITIS B: THE LEADING CAUSE OF MOST LIVER DISEASES
As scaring as it may sound, Hepatitis B diseases is one of the most causative agent of Liver diseaes. Hepatitis B is an infectious disease caused by the Hepatitis B virus (HBV) that affects the liver and can cause both acute and chronic infections. Symptoms may appear 30 to 180 days after infection, with symptoms lasting for a few weeks or up to six months. Acute HBV infections are rare, while chronic ones are more common in those infected at a younger age.
MODE OF TRANSMISSION OF HEPATITIS B
The virus is transmitted through exposure to infectious blood or body fluids, with most cases occurring around birth or childhood contact. Risk factors include working in healthcare, blood transfusions, dialysis, living with an infected person, traveling in countries with high infection rates, and living in institutions. Tattooing and acupuncture were once common but have become less common due to improved sterilization.
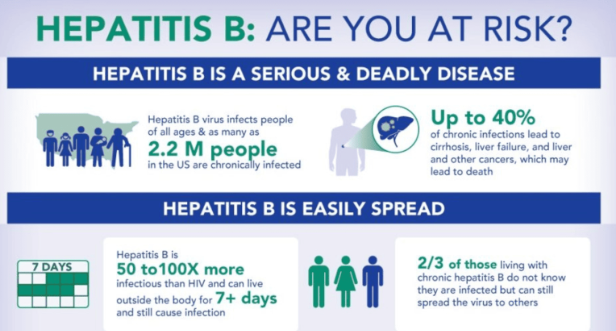
Hepatitis B cannot be spread through hand contact, sharing eating utensils, kissing, hugging, coughing, sneezing, or breastfeeding. The infection can be diagnosed 30 to 60 days after exposure, usually confirmed by testing the blood for parts of the virus and antibodies against the virus. In cases of chronic disease, antiviral medication may be useful, but these drugs are expensive. Liver transplantation is sometimes recommended for cases of cirrhosis or hepatocellular carcinoma.
Vaccination has been preventable since 1982, with the hepatitis B vaccine being between 98% and 100% effective in preventing infection. The WHO recommends testing all donated blood for hepatitis B before using it for transfusion, using antiviral prophylaxis to prevent mother-to-child transmission, and following safe sex practices. By 2030, the WHO aims to eliminate viral hepatitis as a threat to global public health.
SIGNS AND SYMPTOMS OF HEPATITIS B
Hepatitis B virus infection is a severe viral hepatitis that can cause general ill-health, loss of appetite, nausea, vomiting, body aches, mild fever, and dark urine. It can be asymptomatic or asymptomatic and may go unrecognized. Chronic infection can be asymptomatic or associated with chronic liver inflammation, leading to cirrhosis over several years. This type of infection increases the incidence of hepatocellular carcinoma (HCC), which causes approximately 50% of hepatocellular carcinomas in Europe. Chronic carriers are encouraged to avoid alcohol consumption as it increases their risk for cirrhosis and liver cancer. Symptoms outside of the liver are present in 1-10% of HBV-infected people, including serum-sickness-like syndrome, acute necrotizing vasculitis, membranous glomerulonephritis, and papular acrodermatitis of childhood. HBV-associated nephropathy is more common in children, and membrane glomerulonephritis is the most common form. Other immune-mediated hematological disorders, such as essential mixed cryoglobulinemia and aplastic anemia, are not as well-defined and should not be considered etiologically linked to HBV.
HEPATITIS IS A VERY SCARY AND DANGEROUS LIVER THREAT. EARLY TESTING AND DIAGNOSES SAVES LIVES
TAKE ACTION NOW! EARLY TESTING SAVES LIFE!! CLICK THE LINK NOW!!!
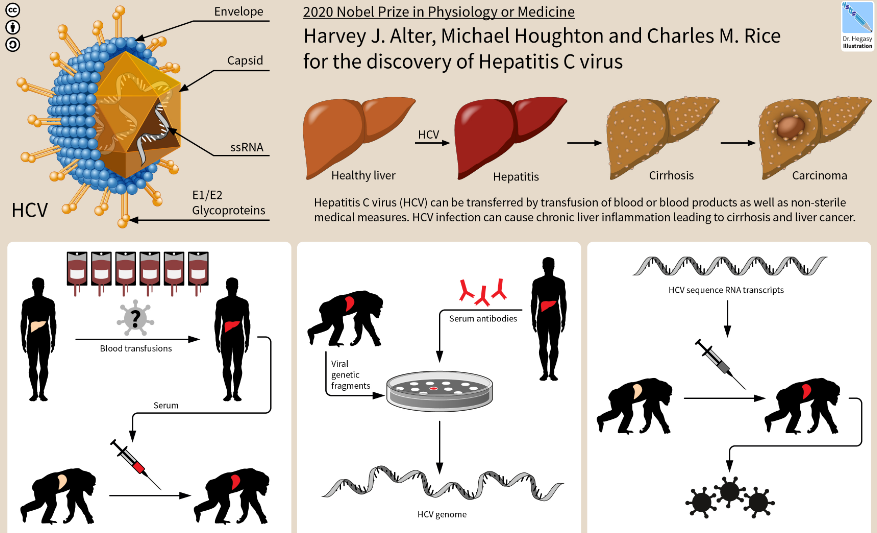
HEPATITIS C: THE LEADING CAUSE OF MOST LIVER DISEASES

Hepatitis C is a viral hepatitis that primarily affects the liver and is spread through blood-to-blood contact, injection drug use, poorly sterilized medical equipment, needlestick injuries, and transfusions. Early symptoms can include fever, dark urine, abdominal pain, and yellow tinged skin. Over time, chronic infection often leads to liver disease and cirrhosis, which can result in serious complications like liver failure, liver cancer, or dilated blood vessels in the esophagus and stomach.
HCV is one of five known hepatitis viruses: A, B, C, D, and E. Diagnosis is by blood testing for antibodies to the virus or viral RNA. In the United States, screening for HCV infection is recommended for all adults aged 18 to 79 years old. There is no vaccine against hepatitis C, but prevention includes harm reduction efforts, testing donated blood, and treatment of chronic infection. Antiviral medications like sofosbuvir or simeprevir can cure chronic infection more than 95% of the time.
In 2019, an estimated 58 million people worldwide were infected with hepatitis C, with 290,000 deaths from liver cancer and cirrhosis. Hepatitis C infects only humans and chimpanzees.
SIGNS AND SYMPTOMS OF HEPATITIS C
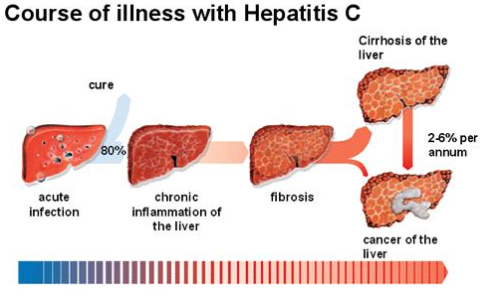
The signs and symptoms of hepatitis are grouped into stages:
ACUTE INFECTION
Acute symptoms of hepatitis C occur in 20% of infected individuals, typically 4-12 weeks after infection. These mild, vague symptoms include fatigue, nausea, vomiting, fever, abdominal pain, decreased appetite, jaundice, dark urine, and clay-colored stools. Acute liver failure is rare, but symptoms and laboratory findings can help diagnose the infection early. After the acute phase, the infection may resolve spontaneously in 10-50% of affected individuals, more common in young and females.
CHRONIC INFECTION
About 70% of those exposed to hepatitis C develop a chronic infection, characterized by detectable viral replication for at least six months. Initially, most experience minimal symptoms but can be associated with fatigue and mild cognitive problems. Chronic infection may lead to cirrhosis or liver cancer. Liver enzymes are normal in 7-53% of cases, but late relapses can be difficult to distinguish from reinfection. Fatigue changes occur in about half of infected individuals, usually before cirrhosis develops. Cirrhosis is more common in those infected with hepatitis B, schistosoma, HIV, alcoholics, and males. Excess alcohol increases the risk of developing cirrhosis 5-fold. Cirrhosis has a 20-fold greater risk of hepatocellular carcinoma, occurring at a rate of 1-3% per year. Liver cirrhosis may lead to portal hypertension, ascites, easy bruising or bleeding, varices, jaundice, and hepatic encephalopathy.
LIVER IS AN IMPORTANT ORGAN AND SHOULD BE HANDLED WITH CARE! AVOID HEPATITIS!! CLICK THE LINK!!!
EXTRAHEPATIC COMPLICATIONS
Hepatitis C is a common cause of mixed cryoglobulinemia, inflammation of blood vessels, and is linked to autoimmune disorders like Sjögren’s syndrome, lichen planus, and insulin resistance. 20-30% of infected individuals have rheumatoid factor antibodies. Other possible associations include Hyde’s prurigo nodularis and membranoproliferative glomerulonephritis. Cardiomyopathy with abnormal heart rhythms is also reported. Chronic infection increases the risk of pancreatic cancer. Other mouth issues include dryness, salivary duct stones, and crusted lesions.
OCCULT INFECTION
Hepatitis C infection can persist even after individuals seem to have cleared the virus. Ultra-sensitive tests can detect the virus, which is not detectable with conventional methods. Newer methods include antibody tests for the virus’ core protein and ultracentrifugation. A form called cryptogenic occult infection has been reported, involving persistently moderately elevated serum liver enzymes without antibodies. This type of infection can be found in people with anti-hepatitis-C antibodies but normal serum levels of liver enzymes, antibody-negative individuals with ongoing elevated liver enzymes, healthy populations without liver disease, and groups at risk for HCV infection. The clinical relevance of this form of infection is under investigation. The rate of occult infection in those seemingly cured is controversial but low.
TAKE CHARGE OF YOUR LIFE! CLICK THE IMAGE BELOW TO SEE MORE!
HIV 1 AND 2
HIV is a retrovirus that attacks the immune system and can be managed with treatment. It is a lifelong regimen of medicine that suppresses the virus, making it undetectable. There is no vaccine or cure for HIV, and an HIV-positive person can expect to live a normal life and die with the virus, not of it. Without treatment, the infection can interfere with the immune system and progress to AIDS, sometimes taking many years. Symptoms may not appear immediately, but they can pass on during a prolonged incubation period with no symptoms. Without treatment, a person living with HIV can expect to live for 11 years. HIV is spread primarily through unprotected sex, contaminated needles or blood transfusions, and mother-to-child transmission during pregnancy, delivery, or breastfeeding. Ways to avoid catching HIV include safe sex, treatment to prevent infection (“PrEP”), treatment to stop infection in someone who has been recently exposed (“PEP”), treating those who are infected,” and needle exchange programs. HIV/AIDS has had a significant impact on society, including discrimination, economic impacts, and religious controversies. In 2021, there were 650,000 deaths and about 38 million people living with HIV, with 20.6 million living with the virus.
SIGNS AND SYMPTOMS OF HIV
MEDICAL DIAGNOSIS EXPERTS HAVE THIS TO SAY:
Early detection saves lives and prevents HIV spread and effect.
If you think you are at risk of getting infected, please consult your physician now. To book an appointment today, please click on the link below:
BOOK AN APPOINTMENT NOW!
HIV remains a significant global health issue, with no universal cure yet. However, advancements in treatment and rare instances of individual cures have been made. Antiretroviral therapy (ART) is the standard treatment, which slows down the virus’s progression and helps people live longer, healthier lives. Scientific research is progressing towards finding a cure, with five confirmed cases of HIV cured. These cases often involve complex and risky procedures, such as stem cell transplants, which are not feasible or safe for all people with HIV. Despite these cases, they provide valuable insights for researchers working on a more widely applicable cure. HIV’s unique ability to integrate its genetic material into host cells makes it challenging to eradicate. It also continually mutates and evolves, making it a moving target for treatments and potential cures. Despite not being curable in the conventional sense, advancements in medical science and research bring us closer to a potential cure.
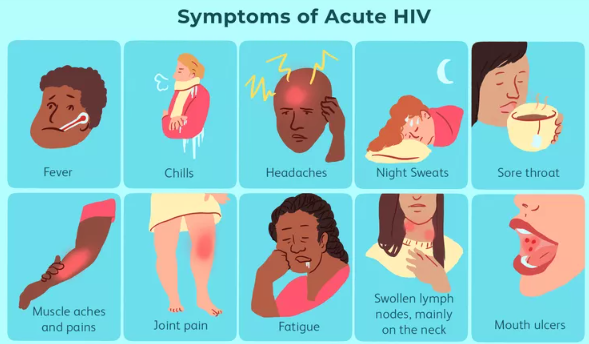
SIGNS AND SYMPTOMS OF HIV
HIV signs and symptoms are categorized in stages of progressions, which include:
FIRST MAJOR STAGE: THE ACUTE STAGE
Acute HIV, primary HIV, or acute retroviral syndrome is the initial period following HIV infection. Symptoms typically include fever, lymph node inflammation, rash, headache, tiredness, and mouth and genital sores. Some cases may develop opportunistic infections. Gastrointestinal symptoms may also occur, and neurological symptoms like peripheral neuropathy or Guillain-Barré syndrome may also occur. These symptoms are not often recognized as signs of HIV infection, and individuals with unexplained fever who may have recently been exposed to HIV should consider testing to determine if they have been infected.